Executive summary
In the 2023 pay negotiations between health unions and the Department of Health and Social Care, the government agreed to ‘work with employers and trade unions to improve opportunities for nursing career progression’ (NHS Employers, 2023). Career progression is an important determinant of job satisfaction and is often associated with an increase in skills, responsibility and autonomy of staff, as well as a movement towards roles that better suit staff. Getting the speed of progression, and the opportunities available to staff, right will be important for retention, recruitment and the productivity of the NHS workforce.
In this report, we examine the career progression of nurses and other staff groups within the NHS Agenda for Change (AfC) pay framework in England over the decade between 2012 and 2021. We document differences in progression across pay bands between staff groups and within groups of nurses to provide important context when considering how – and why – the career progression of nurses needs to be reformed.
To measure the career progression of NHS staff, we use the Electronic Staff Record (ESR), the monthly payroll of all staff directly employed by NHS organisations in England. We define career progression using AfC pay bands. Using pay bands to measure progression captures increases in pay and job responsibilities, but will not capture some other forms of career progression, such as movements between occupations on the same band. We study how quickly new starters in Band 5 (the point at which a newly qualified nurse joins the NHS) progress to Band 6 and beyond. For context, a new nurse starting their career in Band 5 had a basic full-time starting salary of £25,655 in 2021–22. Nurses in Band 6 had a starting basic full-time salary of £32,306 in the same year.
Key findings
1. We create a cohort of nurses who were on the lowest point of Band 5 in November 2012 and record their pay bands over time. By August 2021, 21% of the nurses in this cohort were still in Band 5, 26% were in Band 6, 14% were in Band 7+ and 39% had changed role or no longer worked for an NHS trust. Of those who were still working as a nurse in the NHS nine years after starting, just over one-third (35%) of nurses were still in Band 5 while almost two-thirds (65%) had progressed to at least Band 6.
2. Midwives – by design – progress much faster up pay bands than nurses within the NHS, despite starting at the same pay point. Two years after being at the lowest point of Band 5 in November 2012, among those remaining in the NHS, 8% of nurses were in Band 6+ compared with 84% of midwives. A midwife is therefore over ten times more likely to be in Band 6+ two years after the start of the cohort. By August 2021, 65% of nurses and 100% of midwives were in Band 6+, conditional on remaining in the same staff group in an NHS trust. This may – and of course should – reflect differences in job role and responsibility despite starting on the same band. The NHS Terms and Conditions of Service provides a pathway for staff to progress to Band 6 after two years if their role has sufficient autonomy, and this is currently the case for all midwife roles.
3. While slower than for other staff groups, nurse progression has sped up over a short time. 30% of nurses who were on the lowest point of Band 5 in November 2012 were Band 6+ after four years, conditional on remaining a nurse in an NHS trust, compared with 40% of nurses who were on the lowest point of Band 5 in the November 2016 cohort. A nurse starting in 2016 was therefore one-third more likely to be in Band 6+ after four years than a nurse starting in 2012.
4. There are large regional differences in career progression. A nurse who was at the lowest point of Band 5 in November 2012 was 45% (23 percentage points) more likely to be in Band 6+ nine years later if they started their career in Greater London than if they started in the North East, conditional on remaining a nurse in an NHS trust.
5. Younger nurses are promoted faster to Band 6+ than older nurses. In the November 2012 cohort, 71% of nurses who started aged 20–24 were in Band 6+ by August 2021 conditional on remaining a nurse in an NHS trust, compared with just 45% of nurses who started aged 45+.
6. Male nurses are promoted faster to Band 6+ than female nurses. Among nurses at the lowest point of Band 5 in November 2012, 75% of the men were in Band 6+ by August 2021 compared with 64% of the women, conditional on remaining a nurse in an NHS trust. This may reflect differences in working patterns.
7. There are substantial differences in progression to Band 6+ by ethnicity. Of nurses at the lowest point of Band 5 in November 2012, 67% of White nurses were in Band 6+ by August 2021 compared with 60% of Black nurses and 52% of nurses of Asian ethnicity (and 66% of nurses of Mixed or Other ethnicity), all conditional on remaining a nurse in an NHS trust.
1. Introduction
Career progression is an important determinant of job satisfaction and is often associated with an increase in skills, responsibility and autonomy of staff, as well as allowing staff to move to roles that are better suited to their skills and aspirations. Getting the speed of progression and the opportunities available to staff right will be important for retention, recruitment and the productivity of the NHS workforce.
The career progression of nurses is of particular policy interest. Nurses provide much of the direct clinical care received by NHS patients. They are also one of the largest NHS staff groups: in July 2023, the NHS hospital and community sector in England employed 330,000 full-time-equivalent registered nurses, half of all professionally qualified clinical staff working in the sector and a quarter of all staff working in the sector (NHS England, 2023). In the 2023 pay negotiations between health unions and the Department of Health and Social Care, the government agreed to ‘work with employers and trade unions to improve opportunities for nursing career progression’ (NHS Employers, 2023). Separately, the government committed to explore a separate NHS pay spine just for nursing staff outside of the broader NHS pay framework currently in place (Department of Health and Social Care, 2023).
In this report, we document the progression of new nurses within the NHS over the last decade. This provides important context when considering how – and why – the career progression of nurses could be changed. To do this, we use the Electronic Staff Record (ESR), the payroll of all staff directly employed by the NHS in England. We focus on progression in terms of Agenda for Change (AfC) bands, the pay system used for all NHS employees apart from doctors and very senior managers.
We first document the career progression of new nurses over the first nine years of their career in the NHS. We then examine how nurse career progression compares with that of other NHS staff groups that start at the same pay point – midwives, paramedics and allied health professionals. We also consider how the speed of career progression has changed over time. Finally, we document how nurse career progression varies by the region and trust type where nurses start their careers and by the demographic characteristics of nurses.
This report provides new empirical evidence on the career progression of early-career nurses within the NHS. Throughout, we focus on documenting rather than explaining differences in career progression. Faster career progression for some groups may reflect a quicker or greater accumulation of skills and experience, or more growth in the responsibility and autonomy of their role. It is not possible to determine whether differences in rates of progression are a fair reflection of the different skills and responsibilities required in different roles using our data alone, and we do not attempt to make a judgement on this. But we do highlight where there are differences in progression that might be worthy of further investigation.
The rest of this report is organised as follows. Section 2 describes the NHS pay framework, Agenda for Change, and the data used in the report. Section 3 documents the career progression of nurses and other staff groups in the first nine years of their career. Section 4 shows how the speed of career progression has changed over time. Section 5 shows how nurse career progression varies by the region and trust type where a nurse starts their career. Section 6 shows how nurse career progression varies by age, gender and ethnicity. Section 7 concludes.
2. Background and data
In this section, we describe the Agenda for Change pay system. We then describe the data used to study career progression for different NHS staff groups over time.
Agenda for Change
We measure progression using pay bands within the NHS national pay system, Agenda for Change (AfC). The AfC system was introduced in 2004 and covers all NHS staff apart from doctors, dentists and very senior managers. In March 2023, 1.15 million full-time-equivalent NHS staff in England were employed on AfC contracts (NHS Pay Review Body, 2023).
The AfC pay system is split into nine pay bands, ranging from Band 1 to Band 9, where a higher band is more senior. The band that each role is assigned to is based on the NHS Job Evaluation Scheme. Jobs are assigned points based, for example, on the responsibilities for patient care; on the required knowledge, training and experience; and on the freedom to act (NHS Staff Council Job Evaluation Group, 2020). In general, healthcare professionals with a degree, including registered nurses and midwives, will start in Band 5, with the potential to progress to at least Band 6.
Within each AfC band, there are also pay points (previously called spine points) that staff progress up with experience, conditional on having the requisite knowledge, skills and performance. To illustrate the pay levels of each band, Table 1 shows the lower and upper (basic) pay levels of Band 5 and above for 2021–22. In this year, the entry pay point for nurses and other staff in Band 5 was £25,655, while the highest pay point in Band 5 was £31,534. The entry pay point for staff in Band 6 was £32,306.
Table 1. Agenda for Change basic pay levels in 2021–22
| AfC band | Entry step point | To step point |
|---|---|---|
| Band 5 | £25,655 | £31,534 |
| Band 6 | £32,306 | £39,027 |
| Band 7 | £40,057 | £45,839 |
| Band 8a–8d | £47,126 | £90,387 |
| Band 9 | £93,735 | £108,075 |
Source: NHS Employers, 2021.
The Electronic Staff Record
We use the Electronic Staff Record (ESR) for all analysis in this report. The ESR contains the monthly payroll of all staff directly employed by NHS organisations in England. The data include NHS providers – such as hospital, community and mental health trusts – but do not include primary care staff or staff in contracted-out services. This means that our sample includes all nurses, midwives and allied health professions directly employed by NHS organisations, including those working bank shifts, but does not include those who work in NHS organisations as agency staff.
Each month, the ESR records a range of information about each NHS staff member, including the organisations worked for, hours worked, pay bands, actual pay received and demographic characteristics. We use data between November 2012 and August 2021, which means we can follow the career progression of staff for up to almost nine years. Our sample period includes the COVID-19 period, but we do not focus on the impact of the pandemic on career progression.
The outcomes we consider are whether the staff member is still working in the NHS, whether they are still working in the same staff group, and, if they are still working in the same staff group, their AfC band. One limitation of the ESR is that it does not include staff working at primary care providers, and so we cannot distinguish in the data between staff who have left the ESR data because they have moved to a position within a primary care provider and people who have left the NHS entirely.
3. The progression of nurses relative to other staff groups
We first examine how early-career nurses progress within the NHS. To do this, we create a cohort of all nurses who were employed on the lowest point of Band 5 in November 2012.1 We then track the employment outcomes of each nurse in the cohort over time until August 2021.
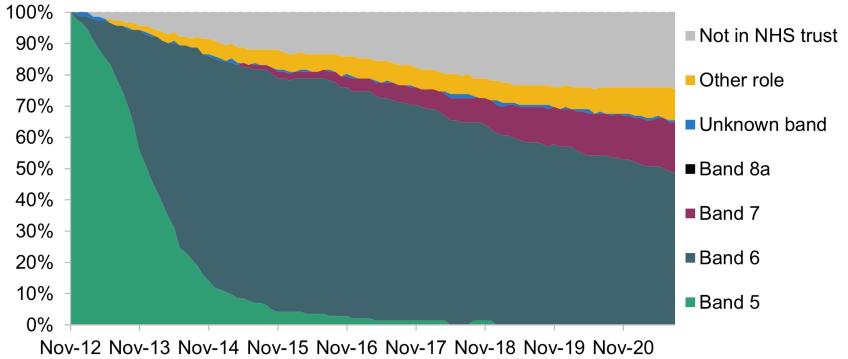
Figure 1 shows the progression of our cohort. The horizontal axis spans November 2012 to August 2021, while the vertical axis is the share of nurses in each outcome group. Each shaded area represents a different outcome listed on the right-hand side, including being in different AfC bands, working in another role and not working for an NHS trust.
Figure 1. Progression of November 2012 nurse cohort
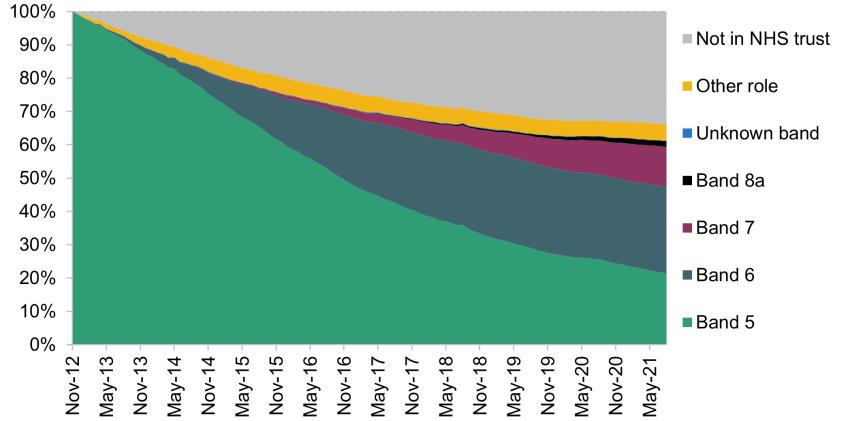
The light green area is the share of nurses working in AfC Band 5. By definition, all nurses in the cohort were in Band 5 in November 2012. Over time, the share of nurses in Band 5 decreased, and by August 2021 only 21% of this cohort were still in Band 5. This decrease is partly because some nurses have been promoted to higher bands and partly because some nurses have changed role or left the NHS. The share of nurses in Band 6 increased gradually over the period. By August 2021, 26% of our cohort were in Band 6, while 12% were in Band 7 and 2% were in Band 8a. Some nurses in our cohort left the NHS (the grey area) or changed their staff role (the yellow area). By August 2021, 5% of our cohort were still working for an NHS trust but not as a nurse, and 34% were no longer working for an NHS trust.
We can also produce this breakdown for other NHS staff groups. In particular, we repeat the analysis for midwives, paramedics and allied health professionals. Allied health professionals are a broad NHS occupation group, and include physiotherapists, radiographers and occupational therapists. We chose these staff groups as, like nurses, these roles require degree-level qualifications and start in AfC Band 5. However, these groups do not have identical roles, and so any differences in career progression may not be surprising given differences in the responsibilities of different roles, despite all starting at the same pay point.
Figure 2 shows the results for each of these staff groups separately. Starting with midwives (Panel A), there is a striking difference in progression compared with nurses. While the share of Band 6 nurses grew gradually over time, the share of Band 6 midwives grew much faster and much earlier. For example, by November 2014, two years after the start of our cohort, 72% of midwives were in Band 6 compared with just 6% of nurses. Even by the end of our period, midwives were much more likely to be in Band 6 than nurses: in August 2021, 49% of midwives were in Band 6 compared with 26% of nurses.
Figure 2. Progression of November 2012 cohorts
A. Midwives
B. Paramedics
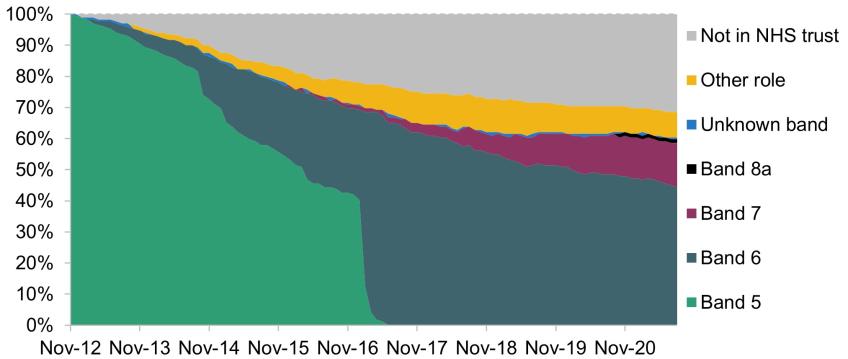
C. Allied health professionals
Annex 20 of the NHS Terms and Conditions of Service provides for some staff groups – explicitly giving the example of midwives – to move to Band 6 within two years of starting their role, if appropriate. The Terms and Conditions justify this based on the autonomy of the roles, typically operating without the influence of other professional groups (NHS Staff Council, 2023) which are reflected in the NHS Job Evaluation national profiles. Roles such as midwives and paramedics often demand a level of autonomous decision-making that exceeds the level associated with Band 5 roles. This would explain why midwives typically move to Band 6 much faster than nurses.
The progression of paramedics (Panel B in Figure 2) was much closer to that of nurses than of midwives for the first couple of years of the cohort. Following a review of paramedic role profiles in 2016–17, a new Band 5 paramedic profile (newly qualified paramedic) and a new Band 6 paramedic profile were developed. These changes saw newly qualified paramedics work for a period of up to two years with additional guidance and support from senior colleagues before moving into a Band 6 role. This was justified as being ‘in recognition of the increasing responsibilities of being a modern paramedic’ (Department of Health and Social Care, 2016) and came alongside a single accredited curriculum for paramedics. By August 2021, no staff in our paramedic cohort were in Band 5 and 44% were in Band 6.
Finally, we consider the progression of allied health professionals (Panel C). Progression for this group was faster than for nurses but slower than for midwives. By August 2021, just 6% were still in Band 5 and 30% were in Band 6.
Table 2 summarises the outcomes of the four cohorts by August 2021. As the previous figures have shown, nurses have the slowest progression of the four staff groups we consider: 21% of nurses were still in Band 5 in August 2021, far higher than the 6% of allied health professionals and 0% of midwives and paramedics.
Table 2. Outcomes of November 2012 cohorts in August 2021
| Band 5 | Band 6 | Band 7+ | Other role / Not in the NHS | |
|---|---|---|---|---|
| Nurses | 21% | 26% | 14% | 39% |
| Midwives | 0% | 49% | 16% | 35% |
| Paramedics | 0% | 44% | 15% | 40% |
| Allied health professionals | 6% | 30% | 23% | 40% |
Many of those in our cohorts left the NHS or no longer worked in the same staff group by August 2021. Table 3 repeats the analysis only for staff who remained working in their role for an NHS trust. The pattern of results is very similar. 35% of continuing nurses were still in Band 5, compared with 11% of continuing allied health professionals and no continuing midwives and paramedics. Correspondingly, continuing nurses were less likely to be in either Band 6 or in Band 7 or higher.
Table 3. Outcomes of November 2012 cohorts in August 2021, conditional on remaining in staff group and working for an NHS trust
| Band 5 | Band 6 | Band 7+ | |
|---|---|---|---|
| Nurses | 35% | 42% | 23% |
| Midwives | 0% | 74% | 25% |
| Paramedics | 0% | 74% | 25% |
| Allied health professionals | 11% | 50% | 39% |
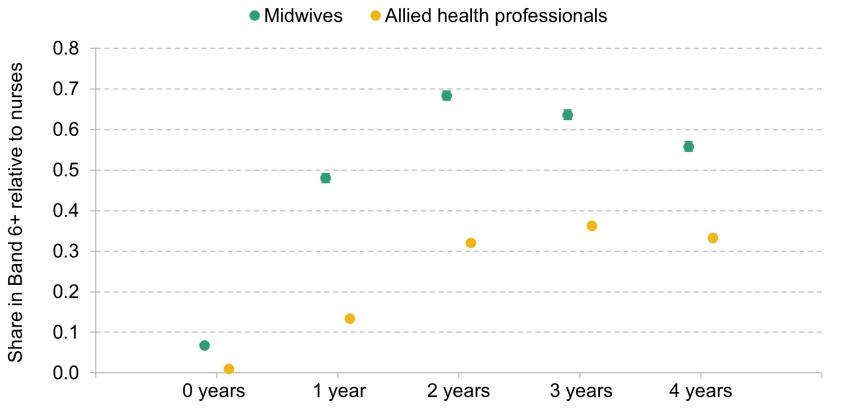
All of our previous analysis has only considered a specific set of cohorts – those that were on the lowest point of Band 5 in November 2012. But these differences in progression by staff group are borne out in other cohorts. In Appendix A, we present regression analysis that combines 56 monthly cohorts of staff starting between February 2012 and September 2016. Consistent with our earlier results, we find that midwives were 79 percentage points more likely to be in Band 6 or above two years after starting, conditional on remaining in the same staff group in an NHS trust. The figure for allied health professionals is 39 percentage points. Figures A1 and A2 in the appendix present the full set of results.
Overall, we find that nurses progress much more slowly up AfC bands than our chosen comparison groups of midwives, paramedics and allied health professionals. Given the way that AfC bands are, at least in theory, determined, this should reflect differences in the roles and responsibilities of nurses relative to these other staff groups. Indeed, the faster progression for midwives is explicitly justified in the NHS Terms and Conditions of Service as relating to the autonomy of their roles. But the change in AfC bands for paramedics in 2016 suggests that the level of progression for different staff groups that is deemed appropriate can change over time.
4. Changes in progression over time
In this section, we consider how career progression for nurses has changed over time. The previous section showed that nurses progress up AfC pay bands at a slower rate than midwives and allied health professionals, but it may be that these gaps have increased – or decreased – over time.
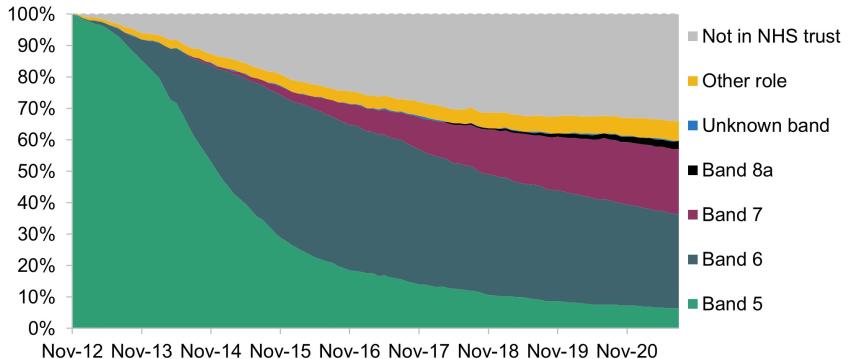
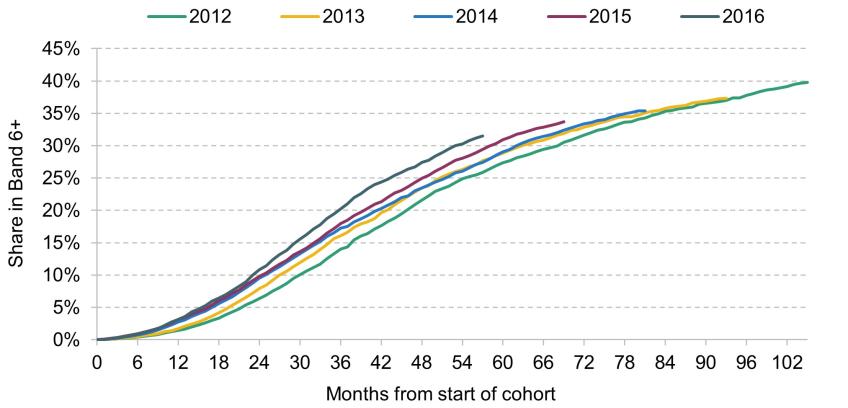
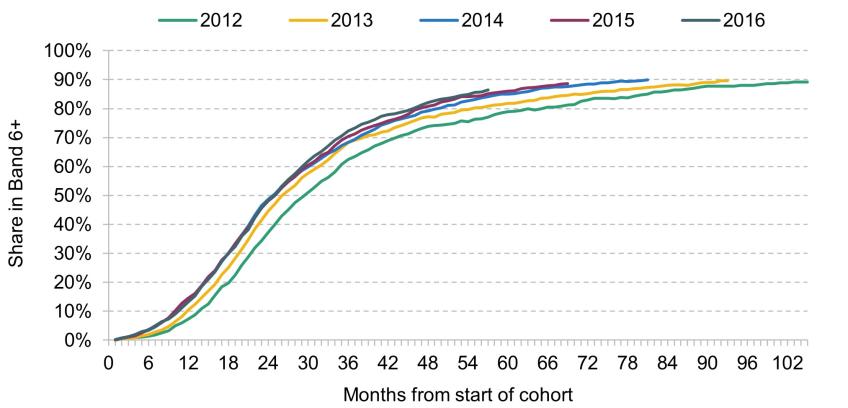
Figure 3 shows how the progression of nurse cohorts has changed between 2012 and 2016. To do this, we form a cohort of nurses starting in November of each year. We then follow each cohort over time until August 2021. Each cohort starts at a different time and runs for a different length, so to compare progression across different cohorts, the horizontal axis shows the months since the cohort started (which will be different calendar dates for different cohorts). The vertical axis shows the share that are in Band 6 or above. Panel A shows results including staff who change roles or who no longer work for an NHS trust (so who are not included as being in Band 6+). Some of these changes in progression over time may be driven by changes in retention of different staff groups over time. Panel B shows results conditional on remaining a nurse working for an NHS trust, therefore removing differences in retention between staff groups and over time.2
Figure 3. Progression of November nurse cohorts between 2012 and 2016
A. Unconditional
B. Conditional on remaining in staff group and working for an NHS trust
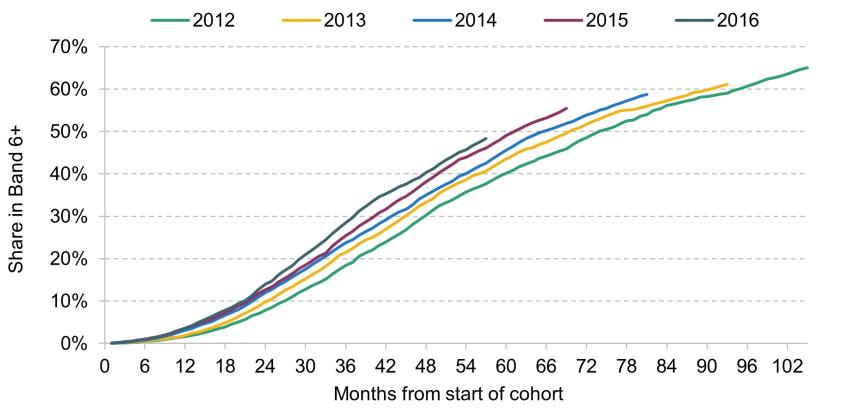
Figure 3 shows that the progression of each nurse cohort follows a similar pattern, but that the speed of progression has increased quite considerably over a relatively short time. Starting with Panel A, four years after starting, 22% of nurses who started in 2012 were in Band 6+, compared with 27% of nurses who started in 2016. Conditional on remaining a nurse in an NHS trust (Panel B), the increase is even larger. Four years after starting, 30% of nurses who started in 2012 and remain working for an NHS trust were in Band 6+, compared with 40% of nurses who started in 2016. This is a very large – 10 percentage point – increase in the speed of progression over just four years.
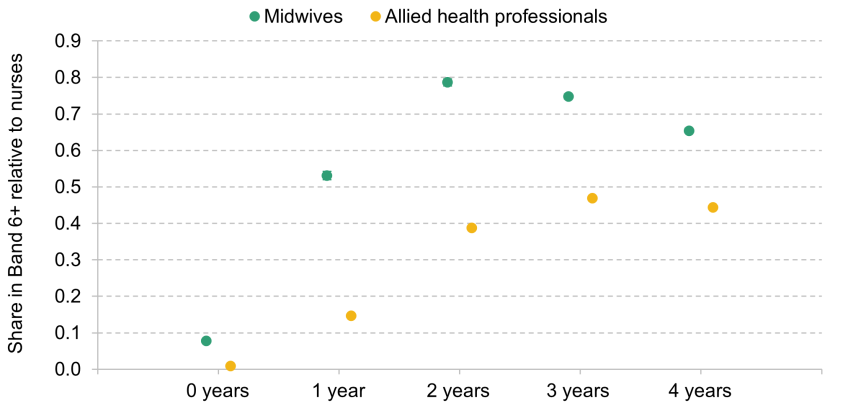
Figure 4 repeats this analysis for midwives. Consistent with our analysis in the previous section, the pattern of progression for midwives is very different from that for nurses, with midwives promoted to Band 6+ much faster than nurses. In Panel A, the share of Band 6+ midwives declines after four or five years because some midwives subsequently stop working for NHS trusts.3
Figure 4. Progression of November midwife cohorts between 2012 and 2016
A. Unconditional
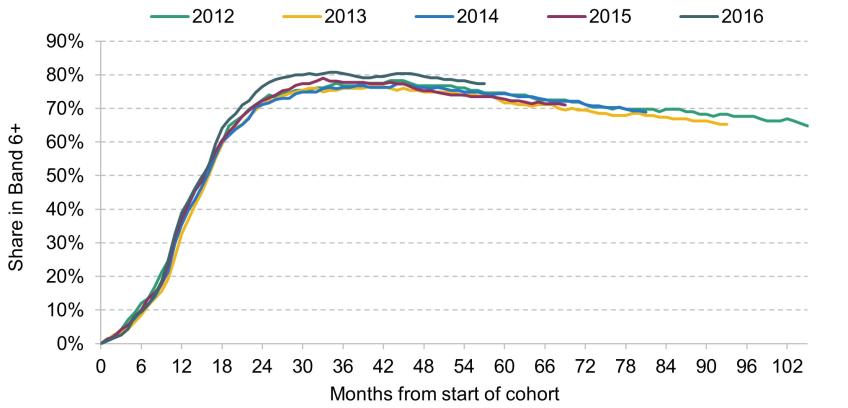
B. Conditional on remaining in staff group and working for an NHS trust
Looking at changes in progression over time, we see that midwife progression has also sped up over time, but at a slower rate than for nurses. Four years after starting, 77% of midwives who started in 2012 were in Band 6+, compared with 79% of midwives who started in 2016. This is a 2.7 percentage point difference, compared with the 5.8 percentage point difference for nurses. But conditional on remaining a midwife in an NHS trust (Panel B), there is almost no difference in midwife progression over time. This is because almost all midwives who remained working for an NHS trust in the 2012 cohort were in Band 6+ after several years, so it is not possible for the share to increase any further.
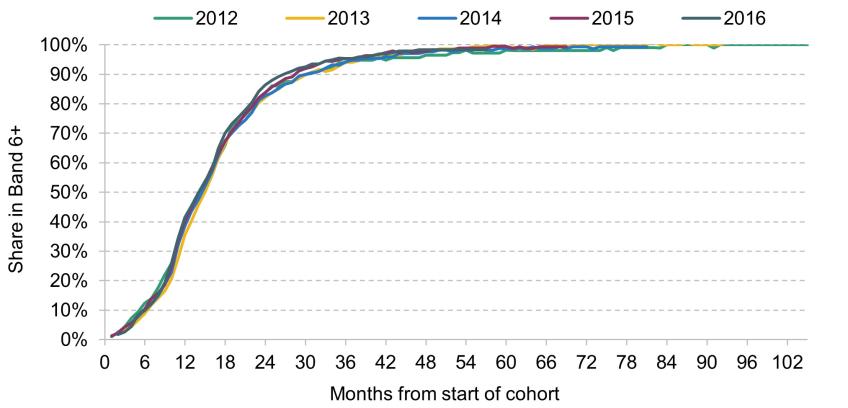
Figure 5 repeats the analysis for allied health professionals.4 The progression of this staff group has also increased over time, similar to the increase for nurses. Starting with Panel A, four years after starting, 53% of allied health professionals who started in 2012 were in Band 6+, compared with 59% of those who started in 2016. Conditional on remaining an allied health professional within an NHS trust (Panel B), the equivalent increase is from 74% to 82%, almost as large as the increase for nurses.
Figure 5. Progression of November allied health professional cohorts between 2012 and 2016
A. Unconditional
B. Conditional on remaining in staff group and working for an NHS trust
Both nurses’ and allied health professionals’ progression has sped up within the NHS over just a short period. There are much smaller changes – if any – for midwives. This means that the gaps in progression between nurses and midwives, for example, are somewhat smaller for those starting in 2016 than for those starting in 2012. But they still remain relatively large: four years after starting in 2016, conditional on remaining in an NHS trust, 40% of nurses are in Band 6+, compared with 98% of midwives.
There are a number of possible reasons that progression within the AfC framework has sped up and we are unable to determine conclusively the cause in this report. It may be that the NHS’s need for more senior staff members has increased over time, or that there are new pathways for staff members to progress faster. One example of a new pathway for progression is the expansion of Advanced Clinical Practice (ACP), which allows experienced nurses and other healthcare professionals to take on more autonomy and responsibility providing care. Equally, it may be that new nurses joining the NHS are now more likely to want to progress to higher bands. But it seems unlikely that these would have changed so dramatically in just four years.
An alternative explanation is that hospitals have increased promotions in an attempt to offset the impacts of NHS pay restraint over this period. When the pay levels at each band are frozen or increase by a small amount, hospitals might respond by increasing their staff’s pay by promoting them up the bands faster in order to retain existing staff and recruit new staff. However, this contradicts the pay progression provisions that applied from April 2021 following the agreement of a new pay progression framework as part of the 2018 AfC pay deal. Although the evidence is only suggestive of this channel, it is consistent with previous work that has found nurses are promoted faster to Band 6 in areas where there are large increases in house prices (Propper, Stockton and Stoye, 2021).
If progression has sped up to offset slow pay growth, this is important and suggests that progression is not just based on the staff mix needs of the NHS and the skills of its workforce, contrary to the design of the pay system. In general, it would be undesirable for career progression to be used solely to increase the pay of the workforce – relative to increasing the pay levels of all or some bands. This is because AfC bands are designed to reflect genuine increases in skill and responsibility, rather than just a desire to pay staff members more.
5. Differences in nurse progression by region and trust type
We now focus on nurse career progression exclusively, and in this section examine differences in career progression by the region and type of trust where a nurse starts their career. Throughout this section, we focus on the November 2012 nurse cohort as this allows us to consider outcomes over the longest horizon.
Region
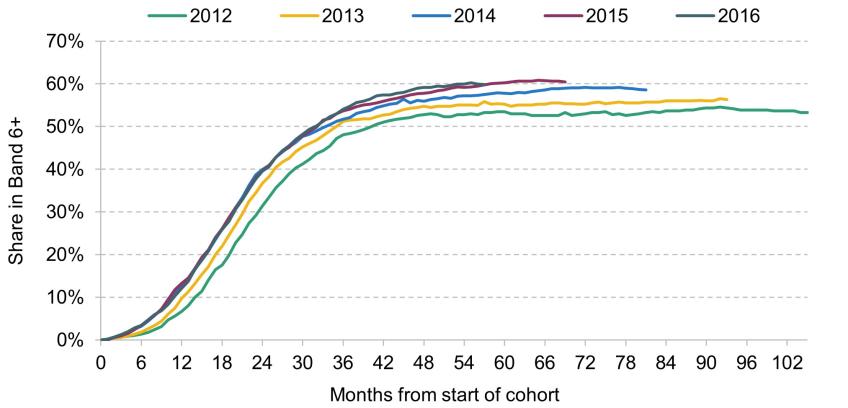
We first consider differences by the region in which a nurse starts their career.5 To do this, we split the November 2012 nurse cohort into nine groups, one for each region of England. Figure 6 shows the progression of nurses in each region. Panel A shows this for all nurses in our cohort, and Panel B shows it conditional on nurses continuing to work as a nurse for an NHS trust.
Figure 6. Progression of November 2012 nurse cohort by starting region
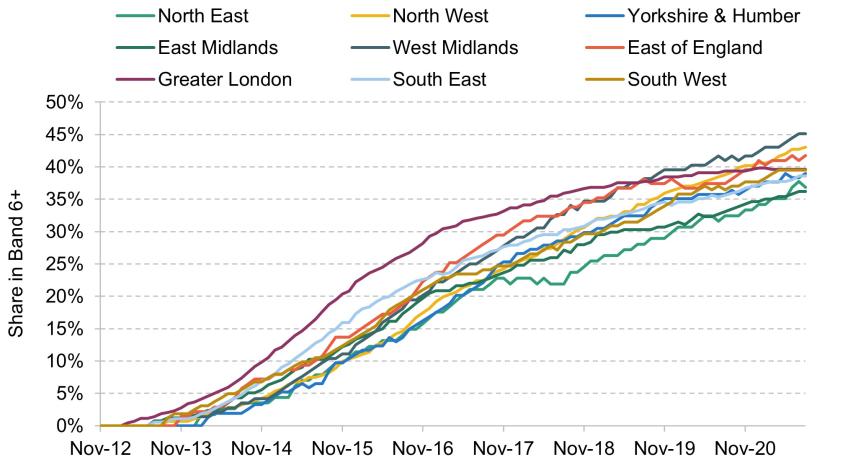
B. Conditional on still working as a nurse within an NHS trust#
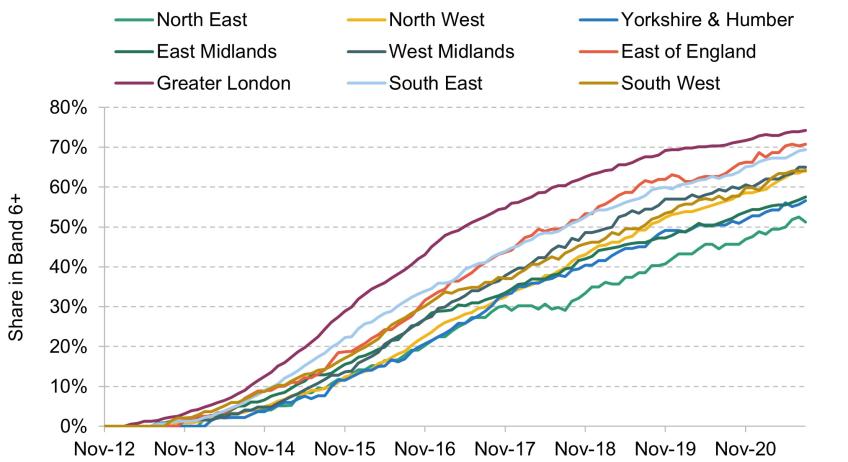
In both cases, there are clearly large regional differences in progression. Panel A shows that, when including staff who no longer work for an NHS trust, Greater London initially has the fastest progression, but is overtaken by the West Midlands by the end of 2019. However, this is largely driven by differences in retention across regions. As Panel B shows, when only including staff who remain as nurses in NHS trusts, Greater London has consistently faster progression than all other regions. For example, by August 2021, 74% of nurses who started in Greater London were in Band 6 or above, conditional on still working as a nurse for an NHS trust.
Greater London is followed by the East of England and the South East, which also have relatively fast rates of progression. At the other end is the North East, with the lowest progression of any region, and Yorkshire & the Humber and the East Midlands. For example, by August 2021, 51% of nurses who started in the North East were in Band 6+, conditional on still working as a nurse for an NHS trust.
These are really large gaps in progression by region. To put it another way, a nurse in our cohort who started in Greater London was 45% (23 percentage points) more likely to be in Band 6+ nine years later than a nurse who started in the North East of England. There are a number of potential reasons for these differences. It may be that Greater London, the South East and the East of England have greater need for Band 6+ nurses than the rest of England, or that the nurses working in these areas are different in some way that means they should be promoted faster. But as with the national increases in progression over time, it may also be the case that progression is faster in these areas to increase pay, perhaps relative to higher outside job opportunities or living costs. Indeed, some suggestive evidence for this explanation is that the three regions with the fastest progression in Panel B of Figure 6 (London, the East of England and the South East) had the highest average wages across all sectors of the economy over this period, while the three regions with the slowest progression (the North East, Yorkshire & the Humber and the East Midlands) had the lowest average wages (Office for National Statistics, 2023).
Trust type
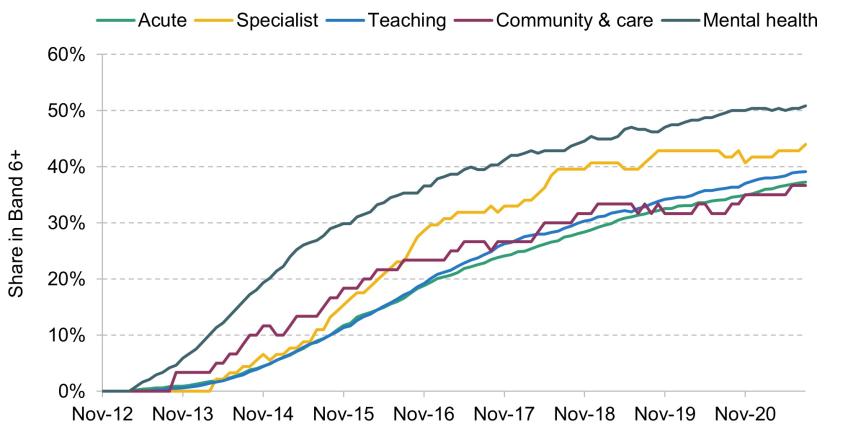
We next consider differences by the type of NHS trust that nurses start in. In particular, we split NHS trusts into five types. Acute trusts are hospitals that provide general acute services. Specialist trusts are hospitals that specialise in particular areas of medicine, such as paediatrics or cancer. Teaching trusts are hospitals that provide general acute services and are also attached to medical schools, and are therefore involved in the training of medical students. Community and care trusts provide care within the community, including district nursing, child health services and social care. Mental health trusts provide services relating to mental health and learning disabilities.
Differences in progression between different types of trusts may exist for a number of reasons. For example, the types of roles and work may differ at different types of trusts, and so there could be different needs for levels of seniority. For example, district nurses employed by community trusts may operate more independently – and perhaps therefore warrant higher pay – than nurses working in acute hospitals on wards with other nurses and doctors nearby.
Figure 7 shows how progression of our November 2012 nurse cohort varies by the type of trust that nurses start in, conditional on nurses staying as nurses working for an NHS trust. Nurses have the fastest progression in mental health trusts, with 82% of nurses in the November 2012 cohort who started in a mental health trust in Band 6+ by August 2021, conditional on remaining a nurse for an NHS trust. Specialist trusts have the next-fastest progression, although this is much slower than for mental health trusts (71% of those who remain in the NHS are in Band 6+ by August 2021).
Figure 7. Progression of November 2012 nurse cohort by starting trust type, conditional on still working as a nurse for an NHS trust
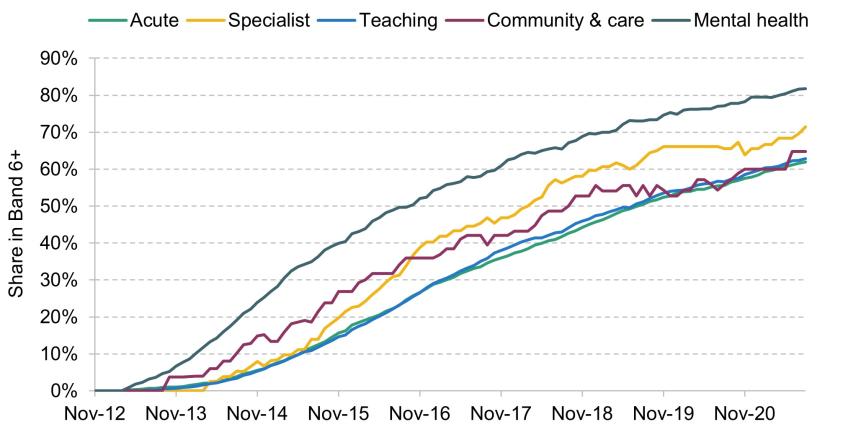
At the other end, acute, teaching and community & care trusts have the slowest rates of progression. For example, 62% of nurses who started in acute trusts and 63% who started in teaching trusts are in Band 6+ by August 2021, conditional on remaining a nurse for an NHS trust.
These patterns, however, are slightly different at the very beginning of nurses’ careers. For example, for the first four years after starting, nurses progress faster in community and care trusts than in specialist trusts, but this pattern is reversed after four years, and specialist trusts have a substantially higher share of nurses in Band 6+ by August 2021 than community and care trusts.
Figure B1 in the appendix repeats this analysis including those who change roles or no longer work for NHS trusts. The pattern of results is very similar.
6. Differences in progression by nurse characteristics
In this section, we examine differences in nurse career progression by demographic characteristics. In particular, we consider differences by the starting age, gender and ethnicity of nurses. We continue to use the November 2012 cohort of nurses in order to study the longest time horizon possible. For each characteristic considered in this section, Table B1 in Appendix B shows the number of nurses in each group.
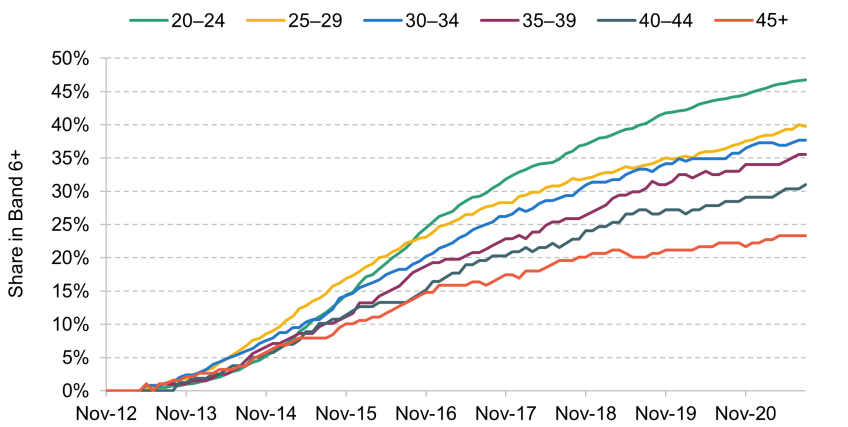
Starting age
We first consider differences in nurse career progression by the starting age of nurses. We might expect differences in progression by age for a number of reasons. Perhaps most obviously, nurses who start at older ages are likely to have larger prior non-nursing labour market experience, which may mean they have greater experience and skills in management and working independently.
Figure 8 shows progression over time for our November 2012 cohort split into six age groups, conditional on cohort members still working as nurses for NHS trusts. At the very beginning of the cohort, nurses aged 20–24 (the group with the most nurses in our cohort) have the slowest rate of progression to Band 6+. But within several years, they have overtaken all other age groups. From four years after the start of the cohort onwards, there is a clear pattern of younger nurses having a higher share in Band 6+ than older nurses. For example, 71% of nurses who started aged 20–24 are in Band 6+ by August 2021 conditional on remaining a nurse in an NHS trust, compared with just 45% of nurses who started aged 45+.
Figure 8. Progression of November 2012 nurse cohort by starting age, conditional on still working as a nurse for an NHS trust
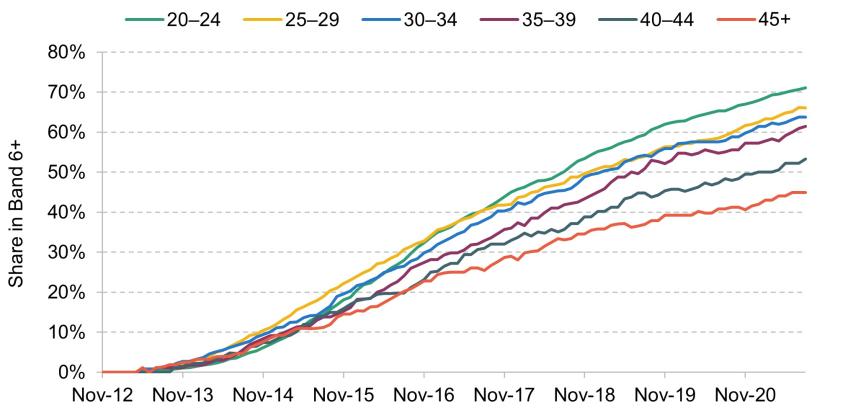
Figure B2 in Appendix B repeats this analysis including nurses who change roles or no longer work for NHS trusts. The pattern of results is very similar.
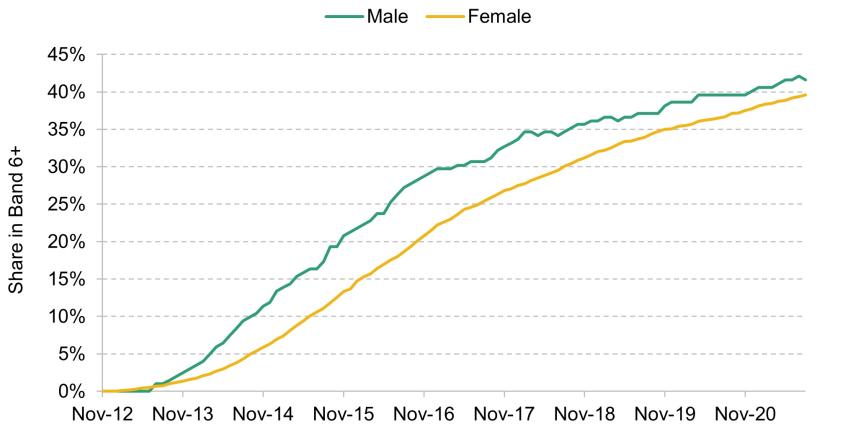
Gender
We next consider differences in nurse career progression by gender. Nursing is very female-dominated, with 90% of the nurses in our November 2012 cohort female. There may be differences in progression by gender if male and female nurses have different experiences or working patterns – perhaps driven by maternity and paternity leaves (Kelly and Stockton, 2023) – different career preferences, or unequal access to training, development or promotion.
Figure 9 shows progression over time for this cohort separately for male and female nurses, conditional on cohort members still working as nurses for NHS trusts (but not on any measure of hours worked or experience gained). The figure shows that male nurses are more likely to progress to Band 6 and above than female nurses. By August 2021, 75% of male nurses are in Band 6+ conditional on remaining a nurse in an NHS trust, compared with 64% of female nurses.
Figure 9. Progression of November 2012 nurse cohort by starting gender, conditional on still working as a nurse for an NHS trust
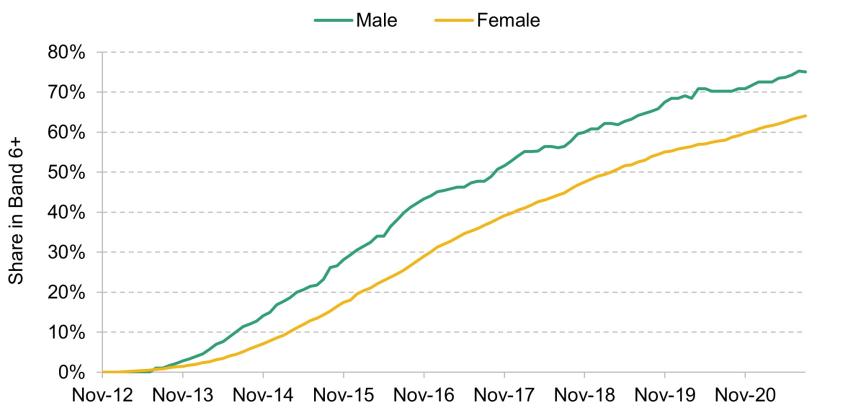
Figure B3 in the appendix repeats this analysis including those who change roles or no longer work for NHS trusts. The pattern of results is similar.
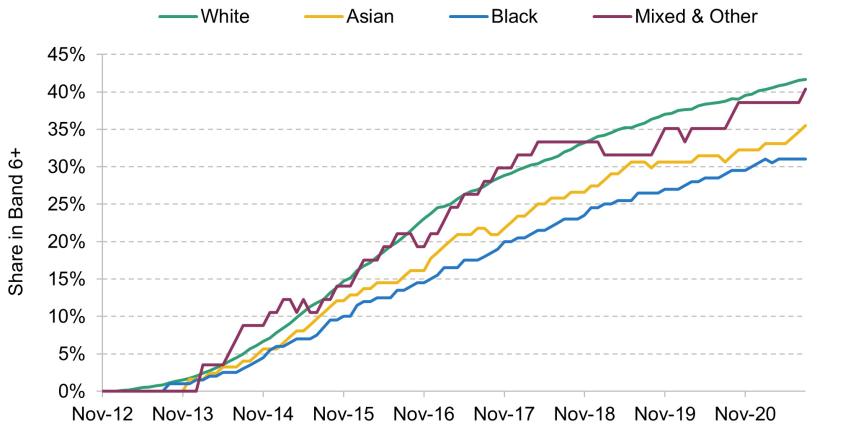
Ethnicity
Finally, we consider differences in nurse career progression by ethnicity. There may be differences in progression by ethnicity for a number of reasons. Nurses of different ethnicities may on average have different educational pathways into nursing, or work in different regions where NHS progression speeds are different. But differences could also occur if there are unequal opportunities for training, development and promotion by ethnicity.
Figure 10 shows progression over time for our November 2012 nurse cohort split into large ethnicity groups, conditional on these nurses continuing to work as nurses in NHS trusts. There are large differences in progression by ethnicity. By August 2021 and conditional on remaining a nurse for an NHS trust, 52% of nurses of Asian ethnicity, 60% of Black nurses, 66% of nurses of Mixed or Other ethnicity and 67% of White nurses are in Band 6+. White nurses are therefore the most likely to be in Band 6+ by the end of our sample period, although nurses of Mixed or Other ethnicity are sometimes more likely to be in Band 6+ than White nurses earlier in their career.
Figure 10. Progression of November 2012 nurse cohort by starting ethnicity, conditional on still working as a nurse for an NHS trust
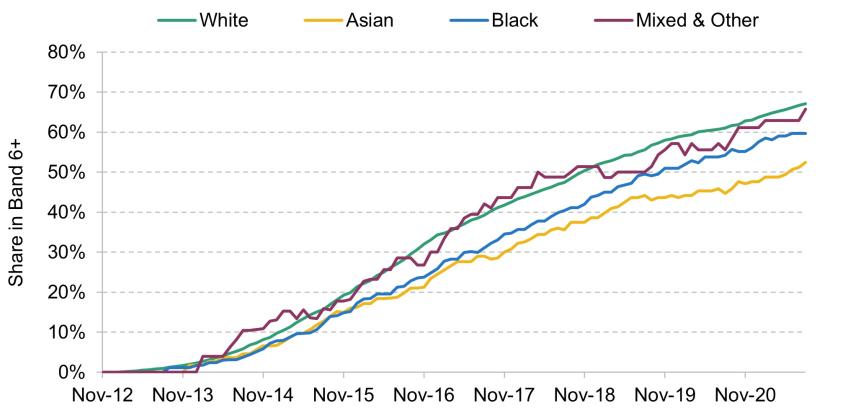
Note: 4.5% of nurses in our cohort had an unknown ethnicity in November 2012 and are excluded. Due to small numbers in each group, we combine Mixed ethnicity and Other ethnicity into one group.
Figure B4 repeats this analysis including nurses who change their role or no longer work for an NHS trust. One major difference between this figure and Figure 10 is for Black and Asian nurses. Conditional on remaining a nurse in an NHS trust, nurses of Asian ethnicity have a lower rate of progression than Black nurses. But including those who leave, Black nurses have a lower rate of progression than nurses of Asian ethnicity. This suggests that Black nurses are more likely to change their roles or no longer work for an NHS trust than Asian nurses.
7. Conclusions
Career progression is an important factor for the pay of nurses, likely to impact retention and recruitment, and an important part of workforce development for the NHS as a whole. In this report, we have documented the patterns of progression along NHS pay bands for early-career nurses in the NHS and how this compares with potentially similar staff groups. Pay bands are an important measure of career progression since they determine the pay that NHS staff receive and they capture changes in job responsibilities. But changes in pay bands will not capture all forms of progression, such as movements between job roles on the same pay band.
We have shown often very large differences in progression between staff groups and between different groups of nurses. Midwives and nurses have similar qualifications and start on the same pay point in the NHS, but within two years almost all midwives have moved to Band 6, whereas very few nurses have. Even after nine years, midwives are much more likely to be in Band 6 or above than nurses. This reflects differences in the responsibilities of the roles, with an expectation that midwives move to Band 6 after two years, as set out in the NHS Terms and Conditions of Service. This is because midwives are assessed by the NHS Job Evaluation scheme to operate with greater autonomy earlier in their career than nurses.
Recent years have seen the speed of progression increase for nurses, with nurses starting in 2016 a third more likely to reach Band 6+ within four years than nurses starting in 2012. Such a large increase over just four years – that was not associated with a large-scale restructuring of roles – suggests that it was not driven exclusively by genuine changes in skills, responsibilities or need for different levels of seniority. Although we cannot say with certainty what has driven this change, one possible explanation is that hospitals have started to promote nurses faster to deal with low national pay growth. This would be consistent with previous findings that hospitals in areas with a larger increase in the cost of living also promote nurses faster (Propper, Stockton and Stoye, 2021). This means that the gap in progression between midwives and nurses has closed, but still remains large.
There are also large regional differences in progression, with nurses starting their careers in Greater London 45% more likely to be in Band 6+ after nine years than nurses in the North East, conditional on remaining a nurse working for an NHS trust. This could be explained by differences in skills or need for types of nurses between regions, but could also reflect the lower relative generosity of NHS pay in Greater London.
Finally, we find that there are differences in career progression by the demographic characteristics of nurses. Younger nurses have faster career progression than older nurses, as do male nurses relative to female nurses. We also find that White nurses tend to progress faster than nurses of Black and Asian ethnicities. All of these differences could be explained by a range of factors, and more research is needed to understand whether they are driven by unequal access to promotion and training opportunities, or whether they reflect differences in skills, experience, location and career preferences across different groups.
Acknowledgements
This research is funded by the National Institute for Health and Care Research (NIHR) Policy Research Programme, through the Policy Research Unit in Health and Social Care Workforce, PR-PRU-1217-21002. The authors also acknowledge financial support from the UK Economic and Social Research Council (ESRC) through the Centre for Microeconomic Analysis of Public Policy at IFS (ES/T014334/1). The authors thank the Department of Health and Social Care (DHSC) for access to data from the NHS Electronic Staff Record (ESR). Figures published using the ESR may be different from the official workforce statistics published by NHS England. The views expressed are those of the authors and not necessarily those of the NIHR, the DHSC or the ESRC.